Improving Traumatic Brain Injury And Burn Care
(SACRAMENTO, Calif.) – The U.S. Department of Defense’s Precision Trauma Care Research initiative has awarded researchers and clinical care specialists at UC Davis Health, and several partner institutions, a 3-year, $4.5 million grant to develop better, more precise treatments for patients who suffer traumatic brain injury (TBI) along with burns or other forms of trauma.
Improve Outcomes
The goal is to improve outcomes for TBI victims by developing a precision medicine approach – a precise, personalized and proactive classification of injury using biomarkers and data – that will enable medical teams to determine the best way to care for patients for improved survival and recovery rates.
“This is a critical project,” said Frederick Meyers, professor of internal medicine and director of the UC Davis Center for Precision Medicine. “The military, for obvious reasons, needs innovations in trauma care in the most challenging of environments, including injury care on the battlefield, in forward-line surgical areas, and in nearby combat-support hospitals. What makes this research doubly important is that the discoveries and breakthroughs we make for our troops can also be applicable back home in the civilian realm.”
Leading Cause of Death
TBI is a leading cause of death in the U.S. military and civilian populations. When combined with burn injury and trauma, such as an explosion or a car crash, traumatic brain injury mortality is doubled. More than 300,000 soldiers have died from TBI in the past 16 years, while approximately 1.5 million Americans sustain traumatic brain injuries each year, with 153 people dying daily from TBI.
The new grant adds to UC Davis’ growing portfolio of Precision Medicine research, which is a relatively new approach to care that allows doctors and researchers to identify and predict more accurately the kinds of treatment and prevention strategies for a particular disease or injury that will provide the best outcomes for specific groups of people or individuals.
Meyers is co-leading the research effort with Tina Palmieri, professor of surgery and assistant chief of burn surgery at Shriners Hospital for Children of Northern California, and other UC Davis colleagues, as well as Major Ian Stewart from the David Grant Medical Center, and Mary Jo Pugh, a University of Utah professor and research health scientist with the U.S. Department of Veterans Affairs.
The Defense Department considers precision medicine to be a very promising approach to injury care. It’s seen as a way to improve outcomes in cases of polytraumatic injury, which occur when a person experiences injuries to multiple body parts and organ systems, often from a blast-related event. Traumatic brain injuries, for example, frequently occur in polytrauma, along with other disabling conditions, such as amputation, spinal cord injury, auditory and visual damages, and burns.
TBI treatments
“TBI treatments usually focus on minimizing intravenous fluid administration to avoid brain swelling, whereas burn treatments use large amounts of IV fluid to replace fluids lost because of the burn wound,” said Palmieri, a nationally recognized burn surgeon and the priniciple investigator on a number of burn studies. “When the two injuries occur together, the question medical teams always face is ‘which strategy should be used?’ We want to develop a good roadmap to navigate the many challenges in these traumatic cases.”
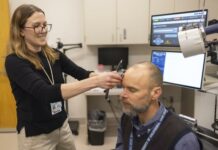
The project is ambitious in its scope and complexity, and it ranges from collecting simple clinical measures such as blood pressure and intracranial pressure readings, analyzing genomic data, gathering advanced monitoring information from electroencephalograms, as well as using evaluation tools such as CT scans.
Assess and Profile
The UC Davis team plans to examine the entire continuum of polytrauma care, incorporating the use of biomarkers, which are measurable indicators of the severity of an injury or presence of disease. This approach can provide a methodical and precise way to identify and characterize clinical conditions such as a traumatic brain injury alone or in conjunction with burns and other trauma injury. By being able to assess and profile TBI pathologies using biomarkers, the team hopes to improve treatment effectiveness and move beyond the traditional ‘one-size-fits-all’ clinical assessments and patient care.
Both Palmieri and Meyers noted that the new project unites experts from a variety of disciplines, many of whom will be working together for the first time. The grant, which was highly competitive, creates a new research network that includes experts from UC Davis’ Regional Burn Center, the university’s departments of emergency medicine, surgery (including trauma and burn specialties), public health sciences, bio-medical informatics and neurological surgery, as well as the West Coast Center for Metabolomics, the Pathology Biorepository and the Center for Genomic Health.
Because of longtime partnerships with UC Davis Health, the David Grant Medical Center at Travis Air Force Base and the Veteran’s Administration are also playing leading roles in the effort.
(21+ years strong)
Welcome to the brighter side!
Get in front of local customers! 24/7 (365)